Abstract

Introduction: the scores APACHE II and SOFA used in Intensive Care Units (ICU) have proven their utility in predicting mortality in critically ill patients. It is classically assumed that the most important prognostic factor in patients with hematological malignancies (HM) requiring admission to the ICU is the underlying disease. The mortality in different series is 44-47%. However, recently studies are evaluating the role of the acute intercurrent disease in the context of HM admitted in ICU since it could be a better predictor of results. Objective: asses the prognostic factors related with ICU's mortality in HM patients.
Materials and methods: retrospective descriptive study of HM patients treated in Hematology Department of Hospital de Clinicas (Uruguay) from 2002 to 2017 admitted in ICU. We evaluated 123 admission episodes in 99 patients. The median age was 57 years old (17-80), 50,5 % were females. The HM were: Non Hodgkin Lymphoma 41,5 %, Acute Myeloid Leukemia 22 %, Multiple Myeloma 11,5 %, Chronic Lymphocytic Leukemia 8 %, Acute Lymphoid Leukemia 4 %, Hodgkin Lymphoma 3 %, Myeloproliferative Neoplasm 3 %, Myelodysplastic Syndrome 2,4 %, aplasia 1,6 %, HPN 1,6 % and Amyloidosis 1,6 %. This study complied with all provisions of the Declaration of Helsinki.
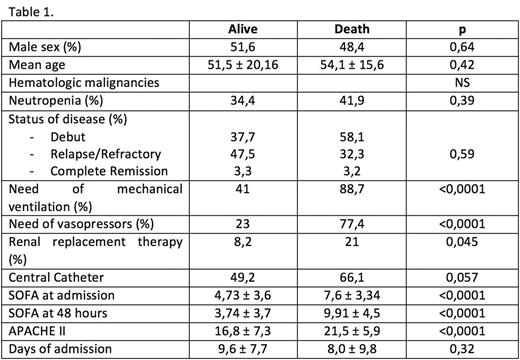
Results: the median duration of ICU stay was 6 days (0-49). Overall mortality was 50,4 %. The main reasons of admission into ICU were: use of mechanical ventilation 43%, clinical monitoring 31%, use of vasopressors 13%, heart monitoring 8% and other 5%. Thirty-eight percent had neutropenia at admission. Infection was the cause of admission in 71% of the episodes: clinically evident without microbiological documentation 32,5%, microbiological documentation without clinical focus 5% and with clinical and microbiological documentation 33,5%. The most important site of infection in this series was neumonia with 41,5%. The type of HM, status of disease and presence of neutropenia did not have an impact in outcome. The use of vasopressors and mechanical ventilation at admission did have an impact in survival. Higher APACHE II and SOFA at admission were related with ICU mortality, p<0,0001. Of the episodes where SOFA was increased in 2 points at 48 hours of ICU hospitalization 87,9 % died. When SOFA did not increase 2 points at 48 hours 73,9 % lived, p<0,0001. In the multivariable analysis SOFA and APACHE II remain independent factors of mortality, OR 1,5 (1,03-2,36) and 1,1 (1,005-1,25). Conclusion: type of disease, remission status and presence of neutropenia did not have impact in mortality. The severity of the acute intercurrent disease measured by APACHE II and SOFA scores did predict mortality in HM patients. This data could better determine which HM patients benefit the most from ICU. Therefore, these parameters should be the ones to be considered at the time of admission into ICU regardless of the subtype and status of disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal